Am I a Candidate for Dental Implants? Key Factors Dentists Look At
If your gums are healthy, your jawbone is strong, and you’re committed to excellent oral hygiene, you’re likely a good candidate for dental implants. It’s that simple. Dental implants aren’t just for a select few; they’re for anyone with a stable foundation and good overall health.
At Barrie Smile Centre, most patients who think they’re “not eligible” are often just a step or two away — sometimes needing only a bone graft or gum treatment to qualify. Thanks to modern imaging and guided surgery, implant success is now achievable for more people than ever before.
Key Takeaways
- Dental implants are a permanent, natural-looking solution for tooth loss, but not everyone qualifies.
- Good candidates have healthy gums, strong jawbones, and excellent oral hygiene.
- Certain medical conditions — like uncontrolled diabetes or heart disease — can increase implant risks.
- Dentists use advanced imaging, such as CBCT scans, to evaluate bone density before treatment.
- Bone grafting may be necessary when jawbone support is insufficient.
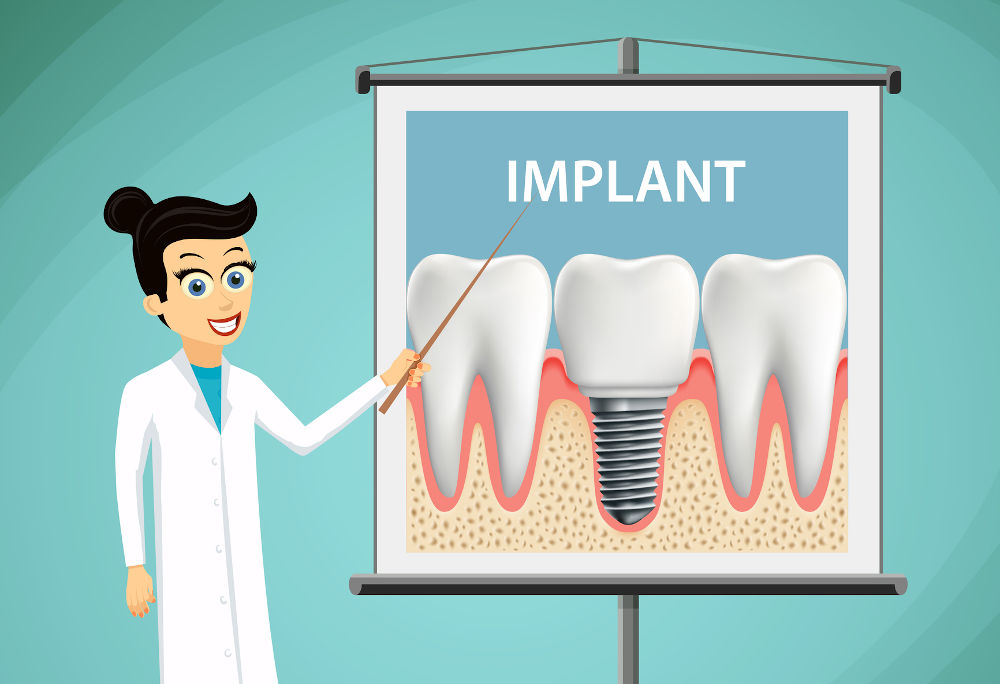
What makes someone a good candidate for dental implants?
Ever wondered why some people qualify for dental implants right away while others need extra preparation? The answer lies in a mix of oral health, bone structure, and overall wellness — not just a missing tooth. Dental implants require a solid foundation, both biologically and behaviourally.
General Health and Oral Hygiene
A person’s overall health is crucial for successful implant placement. Candidates should be free from chronic infections or uncontrolled systemic diseases. Good oral hygiene is essential because implants, though artificial, still rely on healthy gum tissue for stability.
According to the Canadian Dental Association (CDA), poor oral hygiene increases the risk of peri-implantitis — a gum infection that can cause implant failure. Regular brushing, flossing, and dental check-ups are mandatory before and after the procedure.
Gum Health and Bone Density
Healthy gums are non-negotiable. Gum disease or inflammation can jeopardize the implant site. Additionally, jawbone density plays a decisive role. Without sufficient bone volume, the implant can’t fuse (osseointegrate) securely.
When bone loss is detected, bone grafting may be performed before the implant is placed — often a predictable and safe procedure.
Lifestyle Habits
Smoking, heavy alcohol consumption, and bruxism (teeth grinding) can interfere with healing.
Dr. James C.H. Ko DDS emphasizes:
“We look for patients committed to maintaining oral hygiene and lifestyle habits that support healing. Dental implants aren’t a quick fix — they’re an investment in long-term oral health.”
In summary, a good implant candidate maintains excellent oral hygiene, has sufficient jawbone and healthy gums, and is committed to dental maintenance.
Are there medical reasons not to get dental implants?
Even with advances in implant technology, some medical conditions can delay or rule out the procedure. These concerns don’t necessarily mean implants are impossible — but they do require careful management.
Chronic Conditions That Affect Healing
Certain diseases can compromise healing or increase infection risks:
- Uncontrolled diabetes can slow down wound healing and raise infection risks.
- Heart conditions, especially those requiring anticoagulants, may need pre-surgical medical clearance.
- Autoimmune diseases such as rheumatoid arthritis can alter bone metabolism, thereby affecting osseointegration.
- Recent surgeries or radiation therapy to the jaw area can make bone grafting more complex.
Smoking and Dental Implants
Smoking remains a key factor in implant failure. In a 2021 systematic review published in the Journal of Clinical Periodontology, smokers showed nearly double the implant failure rate compared to non-smokers.
Dr. Amir Guorgui BSC, DMD, MACSD, notes:
“We always recommend quitting smoking before implant surgery. It’s not just about improving success rates — it’s about giving the implant the best environment to heal and integrate properly.”
Common Medical Concerns and Dental Implant Considerations
| Condition | Impact on Dental Implant Success | Recommendation |
|---|---|---|
| Uncontrolled diabetes | Delayed healing, higher infection risk | Stabilize glucose before surgery |
| Heart disease | Risk during surgery, anticoagulant interaction | Cardiac clearance required |
| Autoimmune disorders | Reduced bone healing potential | Close coordination with physician |
| Smoking | Higher implant failure rates | Stop at least 2–4 weeks pre-surgery |
| Radiation therapy | Compromised bone quality | Evaluate for grafting or alternative solutions |
When to Proceed with Caution
Patients can still receive implants with these conditions, provided their care is coordinated among their dentist, physician, and, sometimes, a periodontist. What matters most is systemic stability and infection control before surgery.

How do dentists evaluate bone health before recommending implants?
Behind every successful implant is a well-assessed jawbone. Dentists don’t rely on guesswork — they use imaging, measurement, and advanced diagnostic tools to ensure your bone is ready to support the implant.
Role of Jawbone Density
The implant fuses directly into the bone, a process known as osseointegration. This means the bone’s volume and density must be adequate. Thin or porous bone can’t provide long-term stability.
Bone resorption — a common effect after tooth loss — can begin within months, making early evaluation essential.
Imaging Tests: CBCT Scans
The gold standard in dental imaging today is Cone Beam Computed Tomography (CBCT). It creates a 3D model of the jawbone, revealing bone height, width, and density.
At Barrie Smile Centre, CBCT scans are routinely used to plan implant placements with precision, ensuring both function and aesthetics.
Bone Grafting Options
If the scan shows insufficient bone mass, several grafting options exist:
- Autografts (from the patient’s own bone) — most biocompatible.
- Allografts (from a donor source).
- Synthetic grafts (biocompatible substitutes that stimulate bone growth).
Comparison Table — Bone Evaluation and Treatment Options
| Procedure/Test | Purpose | Typical Outcome |
|---|---|---|
| CBCT Scan | Assess bone structure and density | 3D visualization of the implant site |
| Bone Graft | Augment insufficient bone | Restores jawbone volume |
| Sinus Lift | Raise the sinus floor for upper molars | Provides space for implant anchorage |
| Ridge Expansion | Widen narrow ridges | Improves implant stability |
What’s next?
Once bone readiness is confirmed, your dentist develops a customized implant plan — including implant size, angle, and depth — ensuring functional bite alignment and aesthetic harmony.
Who is eligible for same-day dental implants?
Same-day dental implants, also called immediate load implants, allow patients to leave the dental chair with a fully functional replacement tooth the same day their implant is placed. But not everyone qualifies. Eligibility depends on a combination of oral health, bone quality, and lifestyle factors.
Required Criteria: Bone Quality and Gum Health
A strong and dense jawbone is critical for immediate implant stability. Unlike traditional implants, same-day implants don’t have months to fuse with the bone before being loaded with a crown. According to the Canadian Dental Association (CDA), patients must have sufficient bone density and no active gum disease for the procedure to succeed.
Infection-free gums and tissues are non-negotiable. Even minor gum inflammation can interfere with osseointegration. The mouth must be free of decay, periodontal pockets, or other active infections before implant placement.
General Health and Bruxism
Candidates should also be in good general health with no systemic diseases that impair healing. Conditions like uncontrolled diabetes or autoimmune disorders can increase post-surgical risks.
Bruxism (teeth grinding) is another red flag — it exerts excessive pressure on the newly placed implant, increasing the risk of micromovement and early failure.
A study published in the Journal of Prosthodontic Research (2021) found that bone density and occlusal stability (even bite pressure) are key predictors of same-day implant success.
What Patients Say
Patient experiences shared on dental forums like DentalImplantForum.com and RealSelf reflect similar outcomes: those with healthy gums and dense bone report fewer complications, while smokers and those with clenching habits face longer healing times. (RealSelf Dental Implants Review Page)
In short: Good bone, healthy gums, and a stable bite are must-haves for same-day implants.
Can smokers get dental implants successfully?
Smoking is one of the most debated factors in dental implant success. While smokers can receive implants, their long-term success rates are notably lower than those of non-smokers.
Smoking as a Risk Factor
Nicotine restricts blood flow, reducing oxygen delivery to tissues and slowing healing. This directly affects osseointegration — the process by which the implant fuses with the jawbone.
A meta-analysis in the Journal of Clinical Periodontology (2021) reported a 15–20% lower implant survival rate among smokers compared to non-smokers. The risk of peri-implantitis — inflammation and bone loss around the implant — is significantly higher in this group.
Pre-Surgery Requirements
Dentists often require smokers to quit for at least two to four weeks before surgery and remain smoke-free for several months post-surgery. At Barrie Smile Centre, this is standard protocol.
Dr. James C.H. Ko DDS notes:
“The healing phase determines the implant’s future. Even temporary smoking cessation before and after surgery dramatically improves the success rate.”
Smoking and Implant Success Rates
| Patient Type | Implant Success Rate (Average) | Common Complications | Recommendations |
|---|---|---|---|
| Non-smoker | 95–98% | Minimal | Routine hygiene, regular checkups |
| Light smoker (<10/day) | 85–90% | Mild bone loss is possible | Stop smoking 2–4 weeks pre-op |
| Heavy smoker (>10/day) | 70–80% | Peri-implantitis, bone loss | Strongly advised to quit |

What role does age play in dental implant eligibility?
There’s a common misconception that age automatically disqualifies someone from getting dental implants. In reality, age is far less important than bone maturity and overall health.
Age Limitations and Bone Maturity
For younger patients, implants are generally avoided until jawbone growth is complete, typically around 18–21 years old. Placing an implant too early can result in misalignment as the jaw continues to develop.
For older adults, age itself is not a limitation. In fact, research in the International Journal of Oral & Maxillofacial Implants (2020) shows similar success rates in patients over 70 as in younger adults, provided bone quality and systemic health are adequate.
Healing Speed and EEAT Tip
Healing may take longer for seniors due to slower cell regeneration, but the outcomes are equally predictable with careful management.
How does gum disease impact implant success?
Gum disease — or periodontal disease — remains one of the top reasons for implant failure. Before a dental implant can be placed, the mouth must be completely free of infection. Even minor gum inflammation can create major problems once an implant is in place.
Periodontal Disease Risks
Active gum disease weakens the tissue and bone that support teeth. When untreated, bacteria can reach the implant surface, leading to peri-implantitis — a serious infection that mirrors advanced periodontitis. This condition causes inflammation, bone loss, and eventual implant loosening.
Treatment Before Implant Placement
To minimize these risks, gum disease must be treated before proceeding. Treatments include:
- Scaling and root planing to remove plaque and bacteria below the gumline.
- Antimicrobial therapy to reduce infection.
- Bone regeneration or grafting, if bone loss has already occurred.
Reinfection Risk and Maintenance
Even after successful placement, reinfection can occur if plaque control lapses. Daily oral hygiene and regular professional cleanings are critical.
Gum Disease and Implant Outcomes
| Condition | Impact on Implant Success | Prevention/Management |
|---|---|---|
| Active periodontal disease | High risk of peri-implantitis and bone loss | Treat before placement |
| History of gum disease | Moderate long-term risk | Regular maintenance, frequent checkups |
| Healthy gums | Optimal success rate | Maintain a strict hygiene routine |

What are the pros and cons of choosing dental implants over dentures or bridges?
Choosing between dental implants, bridges, and dentures often depends on personal needs, cost, and long-term expectations. Each option comes with unique advantages and trade-offs.
Aesthetic and Functional Benefits
Dental implants mimic natural teeth more closely than any other replacement option. They’re fixed in place, prevent bone loss, and look completely natural. Bridges, by contrast, rely on adjacent teeth for support, which may weaken them over time. Dentures, while affordable, can slip and affect speech and eating.
Durability and Invasiveness
Implants last for decades with proper care. Bridges typically last 10–15 years, while dentures may need to be replaced every 5–8 years. However, implants require surgery, making them more invasive than other options.
Cost Comparison and Long-Term Value
Although implants have a higher upfront cost, their longevity often makes them more cost-effective over time.
Dental Implants vs. Bridges vs. Dentures
| Feature | Dental Implants | Dental Bridges | Dentures |
|---|---|---|---|
| Aesthetic appeal | Natural look and feel | Good, but depends onthe support teeth | Moderate |
| Durability | 20+ years | 10–15 years | 5–8 years |
| Bone preservation | Yes | Partial | No |
| Cost (per tooth) | Higher | Moderate | Lower |
| Maintenance | Routine hygiene | Standard cleaning | Daily removal/cleaning |
| Invasiveness | Surgical | Moderate | Non-surgical |
How long is the recovery process after getting dental implants?
The recovery period after dental implant surgery depends on several factors — including bone quality, the number of implants, and whether grafting was required. While the healing process may take months internally, patients usually resume daily activities within a few days.
Healing Phases
- Initial Recovery (First 48–72 hours):
Swelling and mild discomfort are normal. Patients are advised to rest, avoid physical exertion, and eat soft foods. - Early Healing (1–2 weeks):
Stitches may be removed or dissolve naturally. Any discomfort should subside. - Osseointegration (2–6 months):
The implant fuses with the jawbone during this period — the most crucial phase for long-term success. - Final Restoration:
Once the implant integrates, the permanent crown or bridge is attached.
Aftercare Tips
- Maintain gentle but consistent oral hygiene.
- Avoid smoking and alcohol during recovery.
- Stick to soft, nutritious foods.
- Use a prescribed antimicrobial rinse.
When to Resume Normal Activities
Most patients return to work within 2–3 days, though physical activity should be limited for at least a week. Complete bone integration can take several months — patience during this period pays off in the long term, improving implant strength.
What happens if you’re not a candidate for implants?
Not everyone qualifies for dental implants — but that doesn’t mean a confident smile is out of reach. For patients with limited bone structure, medical contraindications, or budget constraints, several effective alternatives exist.
Alternatives to Traditional Implants
- Dentures: A removable, cost-effective solution for full or partial tooth loss. Modern dentures fit more comfortably and look more natural than older models.
- Dental Bridges: Ideal for patients missing one or two teeth. Bridges rely on adjacent teeth for support, offering a fixed solution without surgery.
- Mini Implants: Thinner and shorter than standard implants, mini implants are often used when bone density is insufficient for full implants.
- Sinus Lift or Bone Graft Preparation: For patients planning future implants, these procedures build sufficient bone mass for later placement.
According to the American Academy of Implant Dentistry (AAID), bone grafting success rates exceed 90%, making it a reliable step toward future implant readiness.
What should you ask your dentist before deciding on implants?
Before committing to implants, a thorough consultation is essential. Knowing the right questions can clarify expectations and prevent complications.
Step-by-Step Guide for Consultations
- Ask about eligibility:
Inquire whether your bone density, gum health, and medical history make you a good candidate. - Request 3D Imaging:
Technologies like CBCT scans reveal bone volume and help plan implant positioning. - Discuss material options:
Titanium vs. zirconia implants vary in biocompatibility and aesthetics. - Understand long-term maintenance:
Ask how to care for your implant and how often checkups are required. - Seek a second opinion if needed:
Reputable clinics encourage second opinions for major dental procedures. - Ask about success rates and warranties:
Top clinics provide transparent data on their implant outcomes.

How does Barrie Smile Centre assess patients for dental implants?
At Barrie Smile Centre, each implant case begins with a personalized, technology-driven evaluation. The goal is precision, safety, and long-term functionality.
Clinic-Specific Assessment Process
- Comprehensive Consultation:
The process starts with a review of medical and dental history to identify any systemic health concerns. - CBCT and Digital Scans:
3D imaging through Cone Beam Computed Tomography (CBCT) and intraoral scans helps map bone density, nerve pathways, and ideal implant placement sites. - Gum and Bite Analysis:
The clinic evaluates soft-tissue health and occlusal stability to ensure long-term stability. - Customized Treatment Planning:
Using digital models, each implant is planned for the perfect balance of function and aesthetics.
Barrie Smile Centre’s Implant Assessment Tools
| Technology/Method | Purpose | Outcome |
|---|---|---|
| CBCT 3D Imaging | Evaluate bone volume and density | Precise implant positioning |
| Digital Impressions | Create a virtual model of teeth | Comfort and accuracy |
| Occlusal Analysis | Assess bite and pressure distribution | Prevents implant overload |
| Gum Health Screening | Detect infection or recession | Ensures long-term success |
Are you a dental implant candidate?
Choosing dental implants is a life-changing decision — but the first step is understanding your personal readiness. Whether you’re eligible now or require preparatory treatment, professional guidance ensures lasting results.
Implant Readiness Checklist
| Evaluation Criteria | Ideal Condition | Next Step if Not Met |
|---|---|---|
| Gum health | No active infection | Treat periodontal disease |
| Bone density | Sufficient jawbone support | Bone graft or sinus lift |
| General health | Stable systemic condition | Physician consultation |
| Lifestyle | Non-smoker, good hygiene | Modify habits before surgery |
| Bite alignment | Stable occlusion | Orthodontic adjustment if required |
Expert Recommendations
- Seek a comprehensive dental evaluation before deciding.
- Consider bone grafting or sinus lift if advised — these procedures often pave the way for successful implants.
- Ask your dentist for their implant success rate and maintenance protocols.
The path to a healthy, confident smile starts with professional insight. With proper assessment and care, nearly anyone can become a strong candidate for dental implants.
Dental Implant Eligibility & Candidacy
How do I know if I’m a good candidate for dental implants?
You’re likely a good candidate if you have healthy gums, sufficient jawbone density, and good overall health. Dentists also assess oral hygiene habits, smoking status, and bite stability. Even if bone loss or gum disease is present, preparatory treatments such as bone grafting or periodontal therapy can often make implants possible.
Can I get dental implants if I have bone loss?
Yes. Bone loss does not automatically disqualify you from dental implants. Many patients successfully undergo bone grafting or sinus lift procedures to rebuild jawbone volume before implant placement. These treatments significantly improve implant stability and long-term success.
Are dental implants safe for older adults?
Yes. Age alone is not a limiting factor for dental implants. Studies show that patients over 70 can achieve implant success rates comparable to younger adults, provided bone quality and systemic health are adequate. Healing may take slightly longer, but outcomes are equally predictable.
Why do smokers have a higher risk of implant failure?
Smoking restricts blood flow and reduces oxygen delivery to healing tissues, which interferes with osseointegration. Smokers have higher rates of implant failure and peri-implantitis. Dentists typically recommend quitting smoking several weeks before and after implant surgery to improve outcomes.
Can dental implants fail even after successful placement?
Yes, though failures are uncommon. Late implant failure is usually linked to poor oral hygiene, untreated gum disease, smoking, or excessive bite pressure (bruxism). Regular dental checkups and proper home care significantly reduce long-term risks.
Are same-day dental implants right for everyone?
No. Same-day implants require excellent bone density, healthy gums, and stable bite alignment. Patients with active infections, insufficient bone support, or teeth-grinding habits may need a traditional staged approach instead.
What happens if I’m not currently eligible for dental implants?
If you’re not eligible right away, your dentist may recommend alternatives such as dentures, bridges, mini implants, or preparatory procedures like bone grafting. Many patients become eligible after proper treatment and healing.

See what our patients are saying:
The Barrie Smile Centre is the best dental office I've ever been to. The staff is very friendly,professional and knowledgeable. They take away any anxiety and fear of going for a procedure. I highly recommend them!
Very clean, professional and friendly! They have done lots of work for me including 2 implants. I highly recommend them!
Very clean, professional and helpful. 2 other dentists previously tried to fix my composite veneer and both times it look awful and/or was the wrong colour. One trip here and everything was fixed!
Very friendly, helpful staff. Makes you feel welcome as soon as you enter. I needed a tooth removed and got in the same day I called. When I arrived I didn’t have to wait. I have numerous problem with my teeth and they came up with a solution. Thank you all so much.
Just got home from the Smile Centre and I'm thrilled with my results. Had Zoom whitening, and it was better than I expected. The attendant took the time to explain everything super thoroughly. She warned I may have sensitivity but so far so good. I wish I did it ages ago.
The first thing I noticed upon entering the building was the beautiful design plan and lovely staff. I was greeted at the door and made comfortable throughout my entire experience. Everything was explained to me in detail and the staff always made sure I fully understood. This is an amazing office and I would 10/10 recommend it!!
Amazing fast clean attentive friendly ! Im sold! Thankkk youuuuu guys !!!!!!! Had a wisdom.tooth taken out under sedation! All.went perfect and you guys were awesomee!
Every time I go to the Smile Centre in Barrie it’s an amazing experience! Everyone from the admin staff to the dentists are so helpful. Not only do they tell you your options (in my case options for a missing tooth), but they also explain the pros and cons of every option. I highly recommend the Smile Centre
Barrie Smile Centre is truly amazing I called and had an issue with with some tooth pain they were able to fit me in same day which I was truly grateful for. All the staff are kind and professional they truly care about there patients. Big thank you to Dr.Eisen for being so kind and helping me in this situation. I highly recommend Barrie Smile Centre 😃 Thanks again
Great family dentist, has always been on time for appointments. Doing a great job during these times with cleanliness as well! Very professional staff!